Claims Specialist
Dempsey Resource Management Inc.
Deskripsi Pekerjaan
Keuntungan
Manfaat yang Diamanatkan Pemerintah
Gaji Bulan ke-13, Dana Pag-Ibig, Liburan Berbayar, Kesehatan Phil, SSS/GSIS
Asuransi Kesehatan & Kesejahteraan
Organisasi perawatan kesehatan
Claims Processing:
· Review and process medical claims submitted by members or healthcare providers.
· Check documents for completeness, including medical abstracts, itemized statements, and official receipts.
· Verify member eligibility, benefits coverage, and policy limits.
· Apply appropriate coding and benefits computation based on the member’s plan and HMO rules.
Data Entry & Record Keeping:
· Encode claims data into the medical claims processing system.
· Maintain updated records of approved, denied, and pending claims.
· Document any adjustments, follow-ups, and discrepancies.
Claims Evaluation:
· Evaluate claims against policy provisions and clinical guidelines.
· Detect potential fraud, abuse, or claim duplication.
· Coordinate with medical providers to validate unclear or questionable claims.
· Accurately calculate payable amounts, co-pays, and exclusions.
Job Position: CLAIMS PROCESSOR/ANALYST
Monthly Salary: PHP 18,000
Work Schedule: Monday to Friday
Working Hours: 8:30 am to 5:30 pm
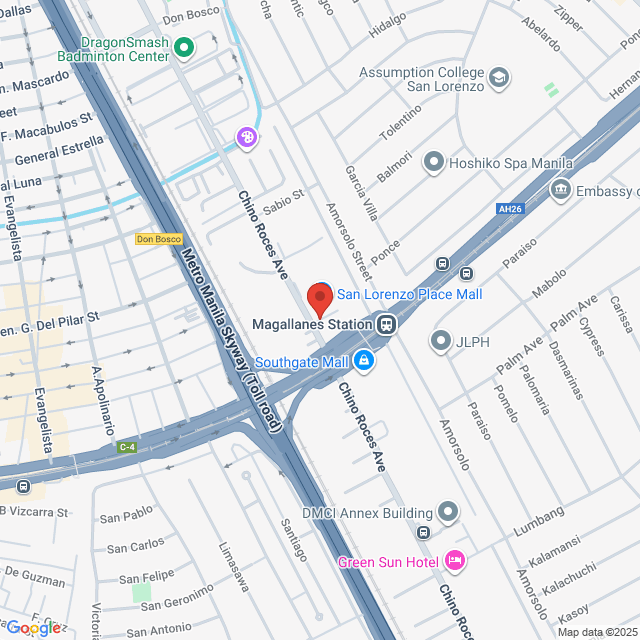
Work Location: Makati Office
Job Qualifications:
Educational Background:
· Bachelor’s degree in Business administration, Healthcare Management, Nursing, or a related field is preferred.
· A diploma in medical, healthcare, or business-related field may be considered.
Experience:
· 1-2 years of relevant experience in medical claims processing or administrative support in healthcare, hospitals, clinics, or insurance/HMO industries.
· Familiarity with medical billing and reimbursement processes.
· Experience working with HMO procedures and healthcare provider networks is a plus.
Skills:
· Attention to Details: Accurate and thorough in reviewing medical claims, documents, and codes.
· Analytical Thinking: Ability to interpret policy coverage, medical reports, and supporting documents to identify discrepancies or irregularities.
· Communication: Strong written and verbal communication skills to coordinate with hospitals, clinics, and policyholders.
· Technical Proficiency: Proficient in medical claims processing systems, Microsoft Excel, MS Word, and email platforms.
· Problem-solving: Capable of investigating claims issues and resolving them in a timely and efficient manner.
Other Qualifications:
· Familiarity with ICD, CPT, and HCPCS codes and medical terminology.
· Knowledge of insurance guidelines, HMO processes, and regulatory compliance.
· Ability to multitask and work efficiently under time constraints.
· Excellent organizational and documentation skills.
HR Vilma Dempsey
Talent Acquisition Manager Dempsey Resource Management Inc.
Balas Hari Ini 0 Kali
Lokasi Kerja
Makati, National Capital Region, Philippines
Diposting di 10 July 2025
Pekerjaan Serupa
Lihat lainnyaClaims Manager
 Manila Bankers Life and General Assurance Corporation
Manila Bankers Life and General Assurance Corporation₺21.8-25.5K[Bulanan]
Di tempat - Makati1-3 Tahun KedaluwarsaS1Penuh waktu

Recruitment opgOwner
Medical Claims Assessor
 Eastwest Healthcare Inc.
Eastwest Healthcare Inc.₺10.9-13.1K[Bulanan]
Di tempat - Makati1-3 Tahun KedaluwarsaS1Penuh waktu

Edlyn SanchezHR Officer
Claims Processor
 Paramount Life & General Insurance Corporation
Paramount Life & General Insurance Corporation₺14.5-18.2K[Bulanan]
Di tempat - Makati1-3 Tahun KedaluwarsaS1Penuh waktu

renee.ursua hrRecruiter
Claims Specialist
 SPD Jobs Incorporated
SPD Jobs Incorporated₺13.8-15.3K[Bulanan]
Di tempat - MakatiLulusan Baru/MahasiswaS1Penuh waktu

Jannelle SombrioRecruitment Supervisor
Claims Specialist
 BPI MS Insurance Corporation
BPI MS Insurance Corporation₺10.9-14.5K[Bulanan]
Di tempat - Makati1-3 Tahun KedaluwarsaS1Penuh waktu

Andres Irad CasidsidHR Manager

Dempsey Resource Management Inc.
101-500 Karyawan
Sumber Daya Manusia
Lihat perekrutan pekerjaan
Bergabunglah dengan Bossjob
Pengingat Keamanan Bossjob
Jika posisi tersebut mengharuskan Anda bekerja di luar negeri, harap waspada dan waspada terhadap penipuan.
Jika Anda bertemu dengan perusahaan yang melakukan tindakan berikut selama pencarian kerja Anda, tolong segera laporkan
- menahan ID Anda,
- mengharuskan Anda untuk memberikan jaminan atau mengumpulkan properti,
- memaksa Anda untuk berinvestasi atau mengumpulkan dana,
- mengumpulkan keuntungan terlarang,
- atau situasi ilegal lainnya.
